Professor Gerald Fogarty is a radiation oncologist in Sydney with an interest in skin conditions.
The purpose of this website is to help patients and their families understand the rationale, process and side effects of radiation treatment of skin conditions, especially through the experience and published work of Prof Fogarty.
Prof Fogarty works at The Icon Cancer Centre at 1-3 MacArthur Avenue, Revesby NSW 2212.
A new patient appointment can be made by calling (+612) 8722 2800 (fax (+612) 02 8722 2801) and asking for an appointment with Professor Fogarty.
More enquires can be made by emailing admin.revesby@icon.team. There is free parking at the nearby Revesby Workers Club.
The Icon Centre at Revesby Centre is 100 metres from Revesby train station, a major railway station on the East Hills line in Sydney.
Prof Fogarty is also on staff at Radiation Oncology, Concord Hospital, Hospital Road, Concord, New South Wales 2139.

Why Choose Radiotherapy
- How Radiotherapy works resulting in tissue conservation
Radiotherapy can treat a mixed population of normal cells and tumour cells, kill the tumour cells but leave the normal cells unharmed. See lip cancer example below.

Large neglected cSCC of Lip 
Six months after Radiotherapy alone 
No surgery was used - Comparison of Radiotherapy and surgery
Definitive radiotherapy is like surgery in that they are both local treatments. They have similar cancer control ability, although further prospective comparative study is required. Radiotherapy is different from surgery in a number of ways. Surgery always removes tissue. Radiotherapy always conserves tissue. Tissue conservation leads to a better functional and cosmetic effect. Tissue conservation leads to better survivorship. Radiotherapy is therefore particularly useful when tissue conservation is important eg face, nose, ears, eyelids, genitals, fingers and toes. RT has no pain on delivery so there is no need for anesthetic. There is no tissue removal, and so no need for grafting, and so no need for an in-patient stay with the leg up for the surgery to heal. As there is no cutting, anticoagulation does not need to be stopped prior to treatment. However, RT is delivered over time and may require many visits. As no tissue is removed there is no histopathology report. There are short term side effects, usually, at the end of treatment, that may require temporary nursing care until healed.
Radiotherapy Surgery Tissue Conservation Yes No Need for anesthetic No Yes Inpatient stay to heal No Yes Stopping Anticoagulation Required No Yes Number of Treatments More Less Histopathology Report No Yes Table comparing Radiotherapy and Surgery - Recent improvements in RT have come from better physics and understanding of radiobiology
Biological improvements allow radiotherapy to kill the tumour cells but leave the normal cells unharmed. Radiation needs to be given in small amounts over time in order to deliver an excellent cosmetic and functional outcome. This is called fractionation. Fractionation describes how the total radiation dose is given in smaller partial doses, often daily. Fractionation allows normal tissue to survive radiation while the tumour cells in the same volume die. This is because normal cells have good radiation repair mechanisms while tumour cells do not. After a small dose of radiation the normal cells can repair while the tumour cells cannot. The tumour cells die. Most repair happens in the first 6 hours following radiation treatment. We are actively researching new biological ways to decrease the number of fractions and therefore decrease the number of visits to the radiotherapy department, to make the treatment experience easier on patients. One of them in mainstream practice now is the Adaptive split course radiotherapy (ASCRT) (Fogarty GB, Br J Dermatol. 2018)
Physical improvements include increased conformity of radiation. Better conformity means that the dose to cancer can be increased while the dose to normal tissue is decreased. Better conformity gives better functional and cosmetic outcomes in normal tissues after treatment. The new technologies deliver enough dose to the skin to cure skin cancer and its precursors, and yet leave the normal skin and organs underneath unharmed.
- The Radiation Treatment Journey
The journey begins with having a consultation with Prof Fogarty. A referral is needed. A new patient appointment can be made by ringing (+612) 8722 2800 and asking for an appointment with Professor Fogarty.The process of having radiation is that there needs to be an initial consultation with myself so that I decide if radiation is the best treatment based on experience and knowledge of the literature. If I think radiation is warranted, I will offer that to you. During the rest of the consultation, I will explain the rationale for treatment, the process and the possible side effects. This is necessary for you to give fully informed consent. You will need to show your consent by signing a treatment consent form. The consent form can be signed by another in charge of your affairs.
The rationale for radiation is the treatment of diseased cells that are mixed in with normal cells. Radiation allows for normal tissue repair of the normal tissue in the volume and yet sterilization of the diseased cells.
Then we get on with the process. First, we organize planning. Planning takes about 1-2 hours. Usually, we can do the planning on the same day as your initial consultation. Planning is aiming the radiation to where it has to go. Planning is not scheduling. Scheduling is when you have the radiation. This should fit your timetable as well as that of the centre.
During planning, you will meet nurses, administration people and our radiation planning staff. You may need a scan. This scan is for planning and not for a diagnosis. No contrast, either by mouth or vein, is needed. You can go home after the scan but we then do a lot of work on the scan. I contour different volumes on the scan. I prescribe radiation to the volumes that include tumour. I show the planners normal tissue volumes that need to be avoided. I approve the plan when there is enough dose going to tumour volumes to control the tumour but the dose to the normal structure is low enough to avoid long term side effects.
The next step in the process after plan acceptance comes treatment. On the superficial machine can start almost immediately with a fractionation pattern that fits in with other responsibilities. The other machines need about a week to plan for. You may even need to come back for a second planning scan if we use a special technique called 3D printed bolus.
I will supervise the treatment and review patients regularly during the treatment in order to make sure the exact amount of radiation is delivered to achieve the best outcomes. During this time, short term side effects may arise eg redness of the skin, flakiness of skin, tiredness, that the doctor will prewarn you about and prescribe medication for any side effects if needed. The nurses will see you regularly and advise on skincare in consultation with me.
There will be a medical follow up a month or two following the treatments and then care will once again be continued by the original skincare doctor who, with the radiation oncologist, forms the skin cancer multidisciplinary team. Medical follow up will examine for disease recurrence or new cancers. We will also look for long term side effects. These are rare especially if we use adequate fractionation.
- Radiation treatment for skin conditions including cancer, pre-cancer or in-situ disease and benign diseases.
Radiation for cancers of the skin
Cancers that can be treated with radiation include basal cell carcinoma (BCC), cutaneous squamous cell carcinoma (cSCC), Melanoma, Merkel Cell Carcinoma (MCC), Lymphoma and a range of rarer tumours such as malignant fibrous histiocytoma (MFH) etc.
BCC and cSCC are sometimes called keratinocytic cancers as they both come from the same cell, the keratinocyte.
All skin cancers that are not melanoma can be described by the term non-melanoma skin cancers or NMSC, but this term is being phased out.Invasive disease is capable of spreading to other organs. The mode of spread can be by local invasion into other organs. This is the usual mode of spread for BCC. It can be by perineural invasion. It can be by lymphovascular space invasion, spreading to nearby lymph nodes, and then into the rest of the body.
Some cancers have a non-invasive phase, also called an in-situ phase. cSCC has various names for its in-situ stage, which include in-situ cSCC, Bowens Disease and intraepithelial carcinoma, they are really all the same thing. Melanoma also has various names for its in-situ stage which include in-situ melanoma, Hutchinson Melanotic Freckle (HMF) and Lentigo Maligna, again really all the same thing. Adenocarcinoma of skin has as its in-situ phase extramammary Paget’s disease (EMPD). The non-invasive phase is considered dangerous as it can progress to invasive disease.
Radiation can be used for benign conditions of the skin
These are not cancer but are troublesome because they have a population of cells that divide regularly when they should not, causing symptoms. Radiotherapy is effective because it slows the pace of cell division.
Benign conditions include Rosacea, Keloid, Psoriasis, Extramammary Pagets Disease (EMPD), hidradenitis suppurativa (HS), Disseminated Superficial Actinic Porokeratosis (DSAP) can be treated with radiotherapy.
Intention of radiation treatment – Definitive, Adjuvant and Palliative treatment settings
Definitive treatment is when radiation is the main treatment. It is usually used alone to cure.
Adjuvant radiation is when radiation is used as a guarantee following another therapy that has unexpectedly not worked well eg RT after surgery when the surgery has not cleared all the cancer.
Palliative treatment is when RT is used to reduce symptoms such as pain, bleeding, the need for dressings, and smell. It stops the cancer having such a great impact on function and cosmesis.
- Radiation treatment and other services at the ICON Revesby Centre
Staffing of ICON Revesby Centre Radiotherapy
A radiation multidisciplinary team made up of doctors, nurses radiation therapist and medical physics all combine to maximize the experience from all angles. All have a specialized role, all are important and you will meet them on your journey. There is a radiation nurse with a specific interest in skin cancer, a radiation therapist also with a specific interest in skin cancer and specific training for that, and a radiation physicist who will help to design the radiation fields and the appropriate filtration needed.
The ICON Revesby Centre has 2 radiation treatment machines specifically designed for skin.
These machines are:

Superficial 300 – Small agile machine specifically designed for skin. It has a range of kilovoltage (kV) energy treatment options. It offers shorter set up and treatment times without the need for significant immobilization devices like masks. Good for the claustrophobic. Patients can be treated in their wheelchairs and beds so there is no need for painful transfers.
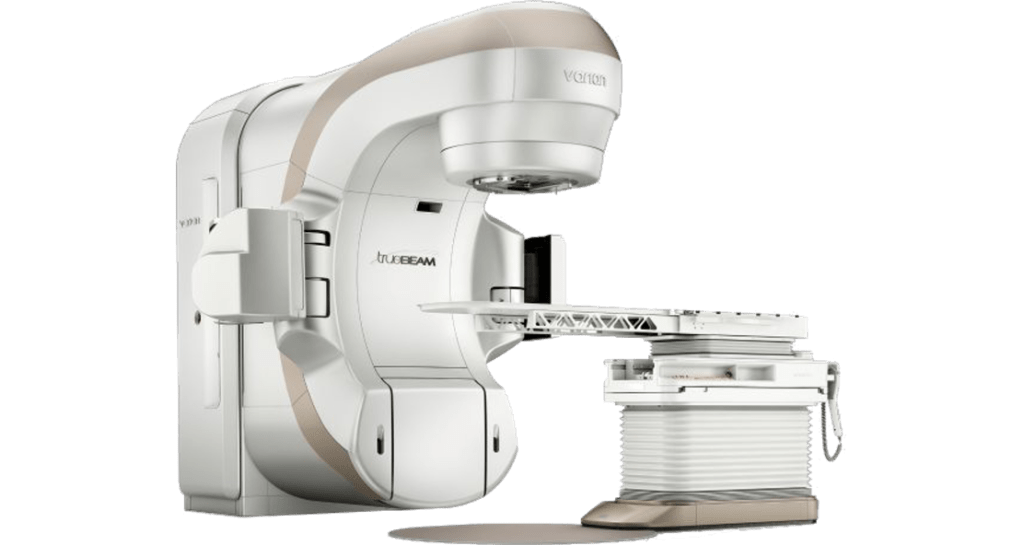
Varian Tru Beam Recently upgraded to deliver better volumetric modulated arc therapy and electron therapies. Electron therapies are excellent for large flat skin surfaces where beam penetration must be kept to a minimum eg large inoperable lesions on lower legs with vascular compromise.
- Skin Biopsy Service at ICON Revesby Centre
Skin biopsy results in a histopathology report from a specialist doctor called a dermato-pathologist. Histopathology via skin biopsy is the gold standard for the diagnosis of skin lesions.
Are you concerned about a skin lesion that is changing but finding it hard to get a biopsy? It can be difficult for busy doctors to have the time to do this. Often patients with serious skin problem have comorbidities that may make a skin biopsy even more time consuming eg anticoagulation, immunosuppression.
Prof Fogarty runs a weekly Skin Biopsy Service at the ICON Revesby Centre.
Punch biopsies are taken under Local Anesthetic. We use a template technique to ensure we track what has been biopsied.